Is Type 1 and Type 2 Diabetes Genetic?

What is diabetes?
Simply put, diabetes is a condition where blood sugar levels increase above normal levels because the body either doesn't make enough insulin or can't use it effectively. The normal range of blood sugar level varies from when you are fasting and rise after meals and is influenced by the composition of the food you eat. The amount of carbohydrates (e.g., in bread, pasta and rice) and in fruits and vegetables, but also the amount and quality of the protein, fat and fibre content which all influence the rate of rise of the blood sugar level in your blood. This rate of rise in blood sugar levels from different foods is known as the glyaemic index or load and it varies between ~ 3.3mmol/L when fasting to as high as 7.8 mmol after eating.
Diabetes can be formally diagnosed with a laboratory blood test ordered by your general practitioner. There are different blood tests to diagnose diabetes:
- Glycated haemoglobin (HbA1c): this non-fasting test is a measure of your average blood glucose over the last three months. It is measured in percent (%) or mmol/mol (millimoles per mole). An HbA1c of 6.5% (48 mmol/mol) or more means diabetes is likely. Between 6.0% to 6.4% indicates pre-diabetes.
- Fasting blood glucose: this test measures how much glucose is in your bloodstream at a certain time of day when you haven’t eaten for eight hours such as overnight. It is measured in mmol/L (millimoles per litre). A fasting blood glucose of 7.0 mmol/L or more indicates diabetes is likely. Between 6.1 mmol/L and 6.9 mmol/L is likely pre-diabetes (also called impaired fasting glucose).
- Non-fasting (or random) blood glucose: this test measures how much glucose is in your bloodstream at a certain type of day if you haven’t been fasting or have eaten something recently. It is measured in mmol/L (millimoles per litre). A random (non-fasting) blood glucose of 11.1 mmol/L or more would indicate diabetes. Between 7.8 mmol/L and 11.0 mmol/L is likely pre-diabetes (also called impaired glucose tolerance).
- Oral glucose tolerance test (OGTT): this test combines a fasting and a non-fasting blood glucose test. After the fasting blood test, you will take a very sweet glucose (75g) drink and your blood glucose will be tested at 1 hour and 2 hours. You are likely to have diabetes if your fasting level is 7.0mmol/L or above, or your 2-hour level is 11.1 mmol/L or above.
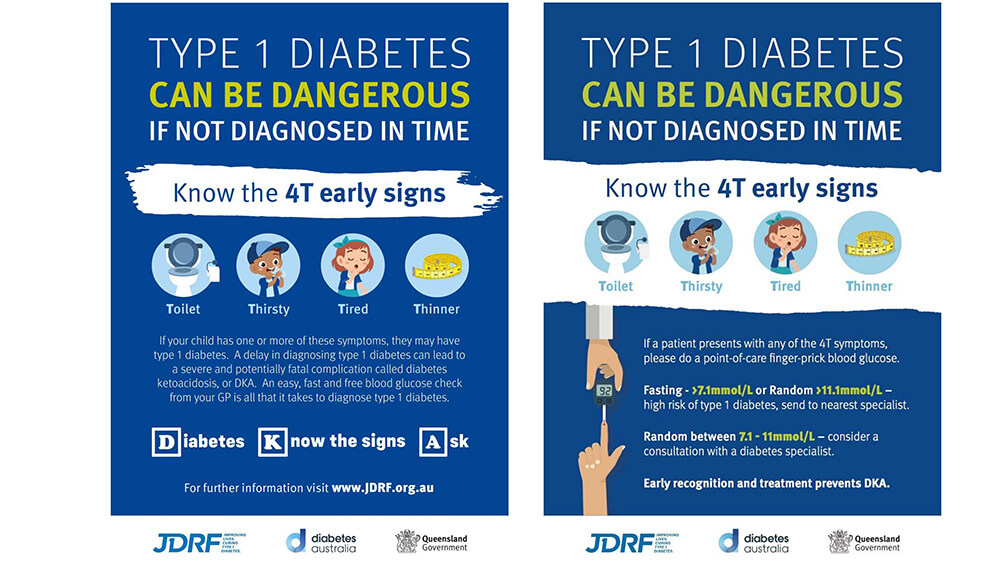
In any child or young adult < 30 years of age a high blood sugar level if fasting > 7.0 and > 11.0 even on a finger prick glucometer reading is serious enough to immediately refer the child or young adult to the local emergency department for an urgent assessment, as they may develop a serious complication of diabetes called Diabetic Ketoacidosis or DKA.
What is the role of insulin hormone in the body?
Produced in the pancreas, insulin is important for managing the levels of sugar (glucose) in our blood. It enables our cells to absorb the glucose through the body for energy, helping our blood sugar levels to stay within a normal range.
In this article, we'll look at the genetic factors linked to Type 1 diabetes and the role environmental factors can play in developing this condition.
What is the difference between Type 1 or Type 2 diabetes?
Type 1 diabetes is a lifelong condition where the immune system mistakenly silently attacks and damages the pancreas's insulin-producing cells. That is why type 1 diabetes is called an auto-immune condition. Eventually as the number of pancreatic insulin-producing so called beta-cells is too low and the person’s blood sugar starts to rise and rise till they present with symptoms related to hyperglycaemia or high blood sugar levels.
Common initial symptoms of diabetes are the same whether you have type 1 or type 2 diabetes and are due to the high blood sugar levels or hyperglycaemia, but include:
- Frequent and excessive urination, and in children bed-wetting in a previously toilet-trained child
- Nocturia or waking at night to pass urine when this was not happening before
- Extreme thirst due to mild dehydration with a dry tongue and skin due to the excessive urination which can lead a person to start drinking exceptionally large amounts of water from > 3-4 litres a day is not uncommon, even in children.
- Loss of weight which can be very significant despite a good appetite
- Tiredness and lethargy are common. Eventually, the person especially if they have unrecognised Type 1 diabetes due to absolute insulin deficiency are at significant risk of developing DKA so they become increasingly tired, lethargic, and unable to function as they did before at school or during normal sports and or at work.
- Other symptoms included blurred vision as the high blood sugar levels affects the shape of the lens of the eye, girls can get recurrent vaginal fungal (thrush) infections, and both boys and girls can get oral thrush.
The high rates of late diagnosis of Type 1 diabetes in children led to the development of diabetes awareness campaigns with posters for GPs and community health centres and at schools using the 4T symptoms (Thirst, Toilet, Tired, Thinner) to highlight these four common symptoms in infants, children and young adults who may present with Type 1 diabetes.
By contrast, adolescents and adults who develop Type 2 diabetes, often have a strong family history of type 2 diabetes or gestational diabetes in their siblings or parents which is associated with being overweight and obese and is related to unhealthy lifestyle factors and higher ethnic risk. See the amazing International Diabetes Federation World Diabetes Atlas which is updated annually and tells you the state of all forms of diabetes around the globe.
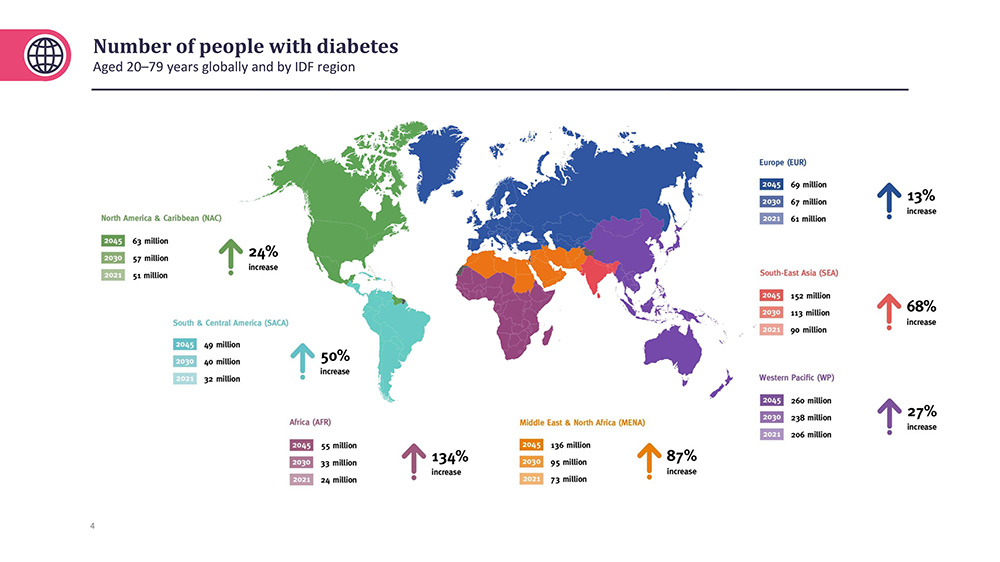
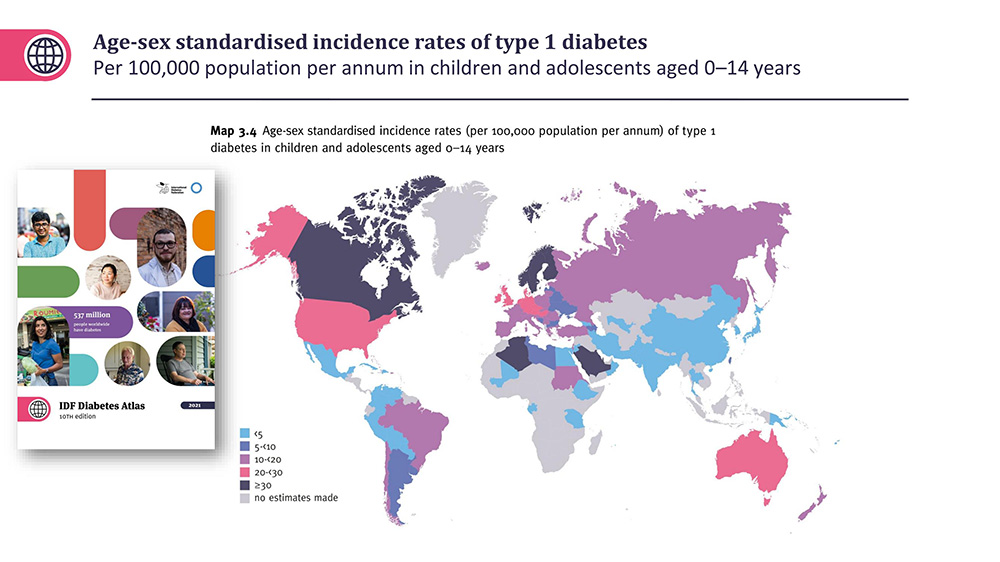
It is frightening to think there are already over 500 million people affected with diabetes which is expected to rise to almost 800 million by 2045. Moreover, a similar number have pre-diabetes, while there are about 1.3 million children around the globe with Type 1 diabetes.
Almost all people with Type 2 diabetes have had warning signs of their diabetes developing for years with weight gain especially round the abdomen, so called visceral intra abdominal obesity which causes insulin resistance and chronic inflammation when cells, particularly muscle, fat and liver cells, don't respond efficiently to insulin.
Eventually the pancreas becomes “exhausted” and the person develops diabetes as the body can no longer continue maintaining the high insulin secretion to keep the person’s blood sugar levels normal.
Type 1 diabetes typically shows up early in life, usually from infancy to early childhood or in adolescence, but can occur later in life in young adults after 30 years of age and has been called LADA for late-onset diabetes in adults.
Unlike Type 2 diabetes, which can be prevented and managed with lifestyle changes, people with Type 1 diabetes require multiple daily insulin injections or the use of an insulin pump to keep the blood sugar levels normal since their bodies do not produce insulin naturally.
Can genes make us likely to develop diabetes?
Our genes play an important role in shaping our health and determining our likelihood to develop certain conditions.
The information encoded in our genes acts as a blueprint for how our bodies grow and work. Certain differences in our genes can increase or decrease the likelihood of developing specific health conditions.
While your genes do play a big part in the risk of developing Type 1 and 2 diabetes, it's important to understand that genes alone aren't the whole story. Type 1 diabetes happens when your genes mix with environmental factors, lifestyle and other to now unknown factors that trigger the autoimmune destruction of the beta insulin-producing cells in the pancreas.
Type 2 diabetes while largely due to lifestyle factors, such as high intake of ultra processed high saturated fat and sugary foods, sedentary behaviour and limited physical activity, combined with important factors like obesity and exposure to certain weight-inducing medications or endocrine-disrupting toxin toxins in the food chain and in air or water pollution, may all play a pivotal role in increasing the risk of developing Type 2 diabetes.
Certain infections and viruses in Type 1 diabetes may also kick-start your immune system into attacking and damaging the cells that produce insulin in your pancreas.
So, even if you carry the genes, you may not develop diabetes unless something in the environment sets it off.
Understanding the relationship between genetics, epigenetics and external factors are crucial for personalised healthcare, as it enables healthcare professionals to identify potential risks and tailor preventive measures and treatments based on an individual's unique genetic makeup.
Why knowing your family's health history matters
If a family member has Type 1 diabetes, it can increase the risk for others in the family. A sibling of a child with Type 1 diabetes has about 8-10% risk of also developing Type 1 diabetes.
Our shared family genes can make us more likely to develop this autoimmune condition so knowing your family's health history becomes important.
It helps you and your healthcare team spot possible genetic factors that could affect your chances of developing Type 1 diabetes.
This awareness is helpful for catching any signs or symptoms early. Regular check-ups and taking steps to prevent problems can be especially good if diabetes runs in your family.
While there is currently no known way to prevent Type 1 diabetes, it can be successfully treated by embracing a healthy lifestyle and effectively managing blood sugar levels.
Eating a balanced diet that limits processed sugars, avoiding smoking, taking regular exercise, and maintaining a healthy weight are some ways to reduce the risk of diabetes complications, such as issues with the eyes, heart, kidneys, nervous system and circulation.
The power of early detection
Early detection is crucial, especially if you have a family history of certain conditions. Knowing your genetic background can provide valuable insights into risks and helps in spotting health issues.
Early detection not only enhances treatment outcomes but also empowers individuals to make informed decisions about their health.
Getting regular check-ups and being proactive based on your genetic background can make a significant difference in how you manage your health, enabling you to take control of your health journey.
For further information about the latest diabetes research to find a cure for Type 1 diabetes go to the JDRF and Trialnet websites.
For further information about Type 2 diabetes, Cardiovascular and Kidney Disease go to either the Baker Diabetes and Heart Disease Institute, the Charles Perkins Centre or NIDDK websites.
Need help to make better lifestyle choices?
November 14th is World Diabetes Day. This WDD the theme is “Know your Risk, Know your Response”. Take the WDD Diabetes Risk calculator checkup - even if you feel it may not help you, it will help your children and your family to know your risk fo diabetes.
If you are worried about your lifestyle choices and the impact they have on your family and your health, we are here to help.
At Childhood Obesity Prevention, we understand that sometimes you and your children may need extra support to make sustainable changes. We have a range of support options available to suit your family, from self-guiding your journey to healthier eating habits with our book Ride to Life, through to personal consultations.
